Episode 106: Psilocybin Therapy - Part 2: Clinical Trials, Secondary Effects, Brain Imaging, and the Future of Psilocybin Therapy
By listening to this episode, you can earn 2.5 Psychiatry CME Credits.
Other Places to listen: iTunes, Spotify
Article Authors: Nadav Klein MD, David Puder, MD
Neither authors have any conflicts of interest to report.
Introduction
With the background from part 1 in mind, in part 2, we review the modern era of research exploring treatment of various psychopathology including depression and anxiety and addiction, the effects on personality, brain imaging and the future of psychedelic research. The results for these studies begin to elucidate the various effects individuals experience with psilocybin. The benefits are potentially impressive, however there are significant limitations that are noteworthy. Psilocybin therapy is just coming out of its nascence, and as with all medicine and therapy it is useful to have a critical view of the research coming out to avoid pitfalls in the future.
Clinical Trials
Depression and Anxiety
The largest number of studies that have been completed have looked at depression and anxiety. We will go through these studies chronologically.
Pilot Study of Psilocybin Treatment for Anxiety in Patients With Advanced-Stage Cancer (Grob et al., 2011)
This is the first study completed in the United States on psilocybin and depression, it was published in 2011:
Participants: A small sample of 12 patients with advanced stage cancer, with a comorbid diagnoses of acute stress disorder, generalized anxiety disorder, anxiety disorder due to cancer, or adjustment disorder with anxiety.
Methods: This was a double-blinded crossover randomized controlled study there was where patients received either niacin or a small-medium 0.2-mg/kg psilocybin dose (for comparison to other trials this was 14mg/70 kg).
Results: There was an overall trend towards significance for improvement of depression and anxiety.
They measured anxiety with self-administered scale, the STAI trait anxiety, which reached significance at the 1-month P=.001) and 3-months (P = .03)
They measured depression using the BDI (Beck-Depression Inventory), a self administered scale, which showed a drop by almost 30% from the first session to 1 month after the second treatment session (P=.05), a difference that was sustained and became significant at the 6-month follow-up point.
Limitations:
There was a small sample size
Expectation bias: it would be easy for participants and providers to determine if the study drug (psilocybin) or the control (niacin) was given
The dose of psilocybin was a small-moderate dose, which did not provide full noetic experience and limits its potential benefit.
Overall there were no adverse events. The general consensus among subjects was that a follow-up experience with psilocybin would reinforce and extend the perceived therapeutic effects of the psilocybin session.
This study was followed by two phase two sister trials that were published side-by-side in 2016 one at Johns Hopkins University and one at New York University.
Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial (R. R. Griffiths et al., 2016)
Participants: 51 participants in various stages of cancer, with comorbid diagnosis of chronic adjustment disorder with anxiety (11 participants), chronic adjustment disorder with mixed anxiety and depressed mood (11), dysthymic disorder (5), generalized anxiety disorder (GAD) (5), major depressive disorder (MDD) (14), or a dual diagnosis of GAD and MDD (4), or GAD and dysthymic disorder (1)
Methods: Embedded within psychotherapy, including preparation and integration sessions. This was a two session, cross-over study with 5 weeks separating the doses with the “placebo” being a low dose (1-3mg/70kg) and the “active dose” being moderate-high doses of psilocybin (30 or 22 mg/kg).
Results:
The overall rate of clinical response (which means >50% reduction of symptoms) at 6 months was 78% for depression and 83% for anxiety.
The overall rate of symptom remission at 6 months for all participants was 65% for depression and 57% for anxiety.
11 of 17 therapeutically relevant measures fulfilled conservative criteria (mostly p < 0.01 and 0.001) for demonstrating efficacy of the high dose of psilocybin for various measurements. Large and significant decreases in clinician-rated and self-rated measures of depression, anxiety or mood disturbance and increases in measures of quality of life, life meaning, death acceptance, and optimism.
There are significant improvements of the high dose compared the low dose with between group effect sizes after session 1 (after 4 weeks): 1.30, 0.81, 0.56, 1.23, 0.60, 0.70, 0.78, 0.65, 0.65, 0.97, and 0.75. Of note, effect sizes are impressive for both the low and high dose of psilocybin, likely indicating a combination of the benefit of therapy, natural changes in depression overtime, and biases.
We can’t say if that’s just because of spontaneous remission because there isn’t a placebo control at 6 months. So, everyone got better, but the problem with a study like this is that we don’t know if they got better because they spontaneously had remission or if they got better because of the treatments or even how much the treatment had an influence.
The study was a cross-over study so there was no control group after the second session. They compared both groups after 6 months to their baseline with extremely impressive effect sizes of: 2.98 for the GRID-HAM-D,1.63 for BDI, 1.65 for HADS depression scale, 3.40 for HAM-A, 1.20 for STAI-strait anxiety, 1.26 POMS total mood disturbance, 1.17 for BSI, 1.14 for MQOL measurement for overall quality of life, 1.12 for MQOL measurement of meaningful existence, 0.84 for LAP-R measure of death acceptance, and 0.66 for the LOT-R measurement of optimism.
For 6 out of 17 scales there were significant changes for both the active and placebo groups between sessions at four weeks, but there were distinguishable no differences between groups. However, when they compared all the participants on these scales at baseline and again at 6 months the effect sizes were impressive: 2.34 for HADS total, 2.15 for the HADS anxiety scale, 1.25 for the STAI State anxiety, 0.58 for death transcendence scale, 0.85 for Purpose in Life Scale, and 0.90 for the LAP-R Coherence scale.
Death transcendence and purpose in life were not different between groups. Considerations for this similarity might be that the improvement came from the therapeutic interactions rather than the psilocybin itself.
Limitations
There were a broad set of diagnoses for participants:
chronic adjustment disorder with anxiety (11 participants), chronic adjustment disorder with mixed anxiety and depressed mood (11), dysthymic disorder (5), generalized anxiety disorder (GAD) (5), major depressive disorder (MDD) (14), or a dual diagnosis of GAD and MDD (4), or GAD and dysthymic disorder (1)
Selection bias: Similar to other studies, as the people interested in this study are likely to be keenly interested in the effects of the medication.
Expectancy effect is likely also to be causing a bias given the perceptual changes that are experienced. These studies bed the question: Is there a good placebo possible?
In this study, the control used was a low dose of psilocybin instead of an inert substance, and it is unclear if microdosing has a therapeutic effect. On some of the measures the low dose seems as effective as the high dose, and it may be beneficial.
Poor blinding despite the study design
Because of the perceptual differences that occur with psilocybin this is a recognized challenge, with only a 10-12% error among therapist during low and high dose sessions. Of note: they did not measure if participants could guess which dose they had been given.
Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial (S. Ross et al., 2016)
Participants: 29 patients at various diagnoses and stages of cancer.
Methods: Embedded within psychotherapy, including preparation and integration sessions. This was a two session, cross-over study, with 7 weeks separating the sessions of the placebo (niacin) with an active dose of moderate-high doses of psilocybin (.3mg/kg or 21mg/70kg).
Results: Between sessions, 83% of participants in the psilocybin group (vs. 14% in the niacin first group) met criteria for antidepressant response and 58% in the psilocybin group had anxiolytic response compared to 14% niacin group. The effect sizes were significant at all time points.
At the 6.5-month follow-up (after the cross-over and both groups received psilocybin), antidepressant or anxiolytic response and remission rates were approximately 60–80%.
They measured the level of the mystical experience directly after the session and whether people experience a “complete” mystical experience correlated with change in depression, and anxiety.
In addition to the benefits with depression and anxiety, participants found these sessions impactful in other ways. 52% of participants rated the psilocybin experience either the singular or at least among top 5 most spiritually significant experiences of their lifetimes. 70% of participants rated the experiences as either the singular or top 5 most personally meaningful experiences of their entire lives. 87% of participants reported increased life satisfaction or well-being attributed directly to the experience.
No change was found in the death anxiety scale.
The side-effects from the psilocybin experiences were limited. “In terms of adverse effects (AEs) attributable to psilocybin, the most common medical AEs were non-clinically significant elevations in BP and HR (76%), headaches/migraines (28%), and nausea (14%); the most common psychiatric AEs were transient anxiety (17%) and transient psy- chotic-like symptoms (7%: one case of transient paranoid ideation and one case of transient thought disorder).”
Limitations of this study are similar to the other studies:
It is unclear from the data whether the sustained benefits in clinical outcomes were due to psilocybin alone or some interactive effect of psilocybin plus the psychotherapy.
This was a small sample size that was not nationally representative of the cancer patient population (62% women, 90% Caucasian)
Blinding was limited with staff members correctly guessing the experimental conditions in 28/29 participants (97%).
Follow up of this study was completed in the following study: Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer (Gabrielle I Agin-Leibes et al., 2020)
Participants: 15 of the 16 living participants participated at two time points after their psilocybin sessions at an average of 3.2 and 4.5 years. 71% had cancer in remission, and 29% still with active cancer.
The figures below show the sustained benefits of the single dose psilocybin session embedded within psychotherapy up to 4.5 years after completion of the study. In the images below, closed points represent significant within-subject differences relative to scores at baseline.
Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study(Robin L Carhart-Harris et al., 2016)
Participants: 12 patients with treatment-resistant depression. (this is a more treatment refractory population that the previous two studies.)
Methods: 4 hrs of preparation, two psilocybin sessions with two different doses (10 mg then 25 mg) one week apart, two in-person follow up sessions one the day after the psilocybin session and the second, the week after.
Results: There was a response rate of 67% (n=8) at 1 week after treatment (HAM-D and BDI), with full remission with seven of these eight patients.
58% (n=7) continued to experience clinically significant response at 3 months, and 42% (n=5) remained in full remission.
For all the depression scales there was significant improvement. The participants’ MADRS improved, on average, from 31.0 (moderate-severe depression) to 9.7 (mild depression) within one week of the sessions. This was a similar change to to the QIDS.
In this study, there were no adverse events beyond transient changes during drug experience itself.
Limitations:
This was an open label study with a small sample size.
This study was susceptible to selection and expectancy bias due to the population being self-referred and treatment-seeking population.
The results are only demonstrated over a relatively short follow-up period of three months.
To take a step back, there was a meta-analysis published on the previous four studies.
The experimental effects of psilocybin on symptoms of anxiety and depression: A meta-analysis (Goldberg et al., 2020)
They note that overall there are large effect sizes on the improvements of both anxiety (g = 1.38, 95% CI [0.78, 1.99]) and depression (g = 1.47, [0.72, 2.21]) compared to baseline. When comparing to placebo, effect sizes are smaller (gs = 0.82 to 0.83 for psilocybin vs. placebo), but keep in mind that both groups are receiving the therapy components, highlighting the large effect sizes that psilocybin itself has.
Limitations of these studies:
Small number of studies and small sample sizes throughout
They raise concern for biases, specifically performance bias and detection bias due to lack of complete blinding
The most recent we looked at was published on November 4th, 2020.
Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial (Davis et al., 2020)
Population: 27 adults started the study with 24 participants completing treatment. All participants with moderate-severe major depressive disorder who were not on medications.
Methods: This was a crossover study. All participants received two psilocybin sessions with the first trial being 20 mg/70kg and the second 30 mg/70kg. The control group was comparing the treatment group with a similar group with an 8 week delayed treatment.
Results: In the overall sample, there was clinically significant reductions in depression for 16 participants (67%) at week 1 and 17 (71%) at week 4, and full remission in 14 participants (58%) at week 1 and 13 participants (54%) at week 4 (<7 GRID-HAMD score).
The effect sizes were large at week 5 (Cohen d = 2.2; 95% CI, 1.4-3.0; P < .001) and week 8 (Cohen d = 2.6; 95% CI, 1.7-3.6; P < .001). There were additional effect sizes for PHQ-9 of d= 3.3, for the HAM-A d=2.3, and the STAI-trait d=2.9.
The QIDS-SR documented a rapid decrease in mean (SD) depression score from baseline to day 1 after session 1 (16.7 [3.5] vs 6.3 [4.4]; Cohen d = 3.0; 95% CI, 1.9-4.0; P < .001), which remained statistically significantly reduced through the week 4 follow-up (6.0 [5.7]; Cohen d = 3.1; 95% CI, 1.9-4.2; P < .001)
As with other studies, many participants found these experiences both personally/spiritually meaningful and psychologically challenging.
This study did not publish the long-term outcomes, which continued to show maintenance of the therapeutic benefit of these sessions with 58% of participants continuing to be in remission after 12 months. This data was collected from a lecture given by the paper’s lead author.
Limitations and Critique of this study are similar to the previous studies:
This is an unblinded multimodal treatment (and notable a treatment that people have a strong desire to experience, similar to ketamine where people drop out post randomization in unblinded trials if they do not receive the study drug).
As seen in the study Antidepressants versus placebo in major depression: an overview (Khan & Brown, 2015), we can expect impressive results to have some regression to the mean with larger sample sizes and better blinding.
There is no good placebo being used for psilocybin.
A few years ago, they wanted to use high dose benadryl which can cause hallucinations, but the IRB would not let them. Maybe in the future trials can use better placebos. Maybe THC, ketamine, or benzodiazepines. Maybe future trials can use an active arm, or non-inferiority trial, compared to a partial hospitalization program.
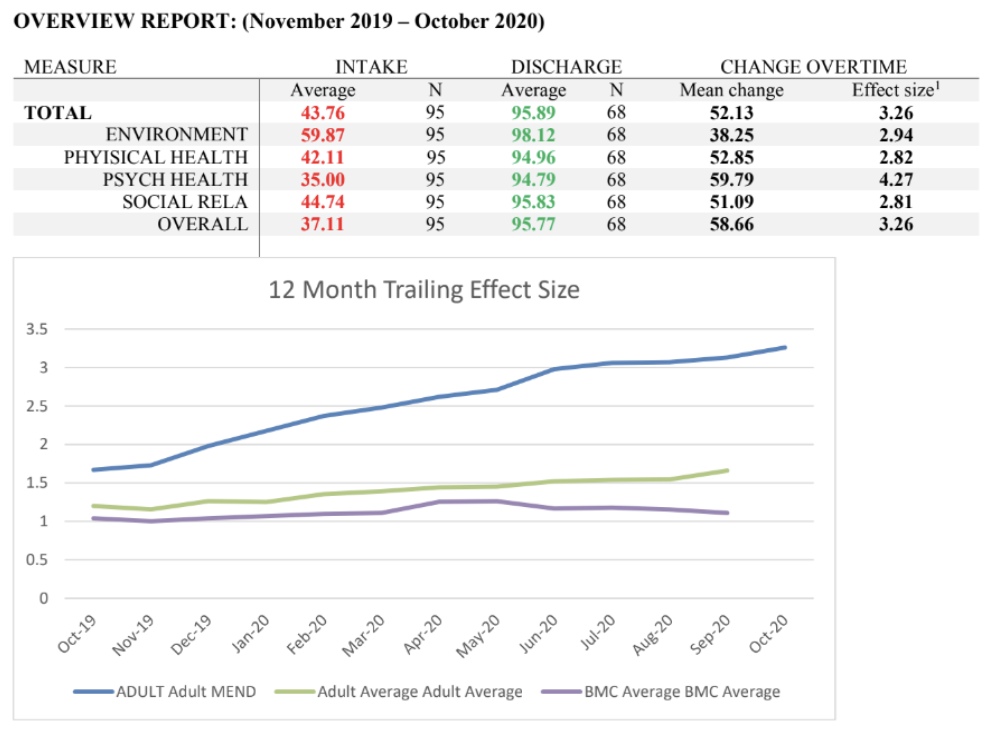
In the partial hospitalization program at Loma Linda, the effect sizes when compared to the general population are similarly impressive with an effect size of 3. There is no control arm, so this is comparing the beginning point to the end point.
Looking at studies can be confusing with different studies measuring their active arm to different control arms. If the control arm is a waitlist, placebo, or active control makes a big difference in the effect sizes. There are differences between industry sponsored vs non-industry vs government sponsored studies. There are effects of having a charismatic leader with top-notch providers. As will providers with an investment in running an experiment.
The variables we choose to control will make a difference. The impact of over-controlling a study will lead to differences in efficacy vs effectiveness. We want to use evidence-based research to translate to real life, but we live in a world with uncontrollable variables.
Other psychiatrists who look at this study wonder if people would malinger to get this type of treatment, similar to ketamine where people dropout post randomization in unblinded trials if they did not get into the ketamine arm of the study.
Another critique to be aware of when assessing this study, is if you looked at early studies with Brexanalone, from the pilot paper, the effect size was more than 1. But, in phase 3 of the study, Sage didn’t publish it because the effect size was so small. Could the effect size of psilocybin change in a multi-center study?
Addiction: Nicotine and Alcohol
Psilocybin-assisted psychotherapy has been used for the treatment of substance use, demonstrating efficacy in a few pilot studies.
Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction.(Johnson et al., 2014)
Population: 15 participants (10 men + 5 female, 5 hallucinogen naive). All participants were motivated to quit, had a history of smoking for an average of 31 years, with a mean of 6 failed past attempts.
Methods: Psilocybin sessions were integrated with smoking cessation CBT. They had 3 psilocybin sessions, the first session was done with a moderate dose of 20mg/kg then two sessions with a higher dose of 30mg/kg unless participants opted for the moderate dose
Results: At six months after the psilocybin sessions,12 out of 15 participants were abstinent (80% success). 3 out of 15 participants continued to smoke, but at a reduced rate. Only one participant denied it had been useful.
Eleven (73%) rated at least one of the psilocybin sessions among the 5 most spiritually significant experiences of their lives, and 13 (87%) reported that their personal well-being or life satisfaction had increased very much as a result of at least one of the psilocybin sessions.
Participants reported that the benefits they experienced increased their time horizon (thinking more long-term), increased self-efficacy, and altered life priorities are involved in tobacco cessation.
In a follow up study (Johnson et al., 2017)
Results: At 12-month follow-up, 10 participants (67%) continued to be smoking abstinent. At long-term follow-up, with a mean interval of 30 months (range = 16–57 months), nine participants (60%) were confirmed as smoking abstinent.
Limitations of this study include the sample size, that it was not a randomized study, and the demographics not generalizable to the general population.
Psilocybin-assisted treatment for alcohol dependence: A proof-of-concept study (Bogenschutz et al., 2015)
Participants: 10 patients with alcohol use disorder.
Methods: Open label study with 2 sessions of psilocybin (0.3 (21mg/kg after 4 weeks) then 0.4 mg/kg(28mg/kg after 8 weeks)) integrated as part of a 12-week motivational enhancement therapy.
Results: Significant improvements in reductions of both total and heavy drinking days after psilocybin with large effect sizes (d=.86-1.38)
The decrease was correlated strongly with the intensity of mystical experience as measured by the MEQ30, r=.782-.865
Demoralization
There are very limited psychotherapeutic medications or therapies used to target this population, who tend to be treatment refractory.
Psilocybin-assisted group therapy for demoralized older long-term AIDS survivor men: An open-label safety and feasibility pilot study (Anderson et al., 2020)
Population: 18 participants with moderate to severe demoralization.
Methods: This was a pilot study with three sequential treatment groups of 6 participants per group. Over seven weeks, participants underwent three hours of individual psychotherapy, 12-15 hours of group psychotherapy, and one eight-hour individual psilocybin administration.
There was no placebo group due the difficulty of functional blinding, particularly in population where 7/18 had previous experience with psychedelics
Results: Change in demoralization showed a clinically significant, small-to-moderate effect size worth of improvement comparing baseline to both end-of-treatment and 3-month follow-up with a standardized effect size of ἠp2 = 0.47, 90% CI 0.21-0.60.
88.9% demonstrated at least a 2-point reduction in demoralization compared to baseline at end-of-treatment with 66.7% maintaining those gains at 3-month follow-up. While 50% had a > 50% reduction in demoralization compared to baseline at the end of treatment and 33.3% maintained those gains at 3-month follow up.
They show that group therapy is an effective way to both utilize the group therapeutic dynamic and decrease the potential cost of the psilocybin-assisted treatment.
The group therapy and psilocybin was well-tolerated overall with 14 of 18 participants having some expected side effects.
“One participant with SCID-5 diagnoses of generalized anxiety disorder, panic disorder, and BPD, in addition to decades of heavy polysubstance use, initially experienced significant anxiolysis after his medication visit. However, ten days later he reported severe anxiety, which he described as a deeply felt sense of being rejected by the other group members. He then, after learning that a former partner had suddenly died, had a lapse in his methamphetamine use and cocaine use (after having been sober from all substances for one month prior to the study). As had occurred once previously in his life, he developed a brief psychotic episode subsequent to methamphetamine use. During this episode, the participant made a suicide attempt of actual lethality 0 (No physical damage or very minor physical damage (e.g., surface scratches)) and potential lethality 2 (Behavior likely to result in death despite available medical care) on the C-SSRS. He withdrew from the study intervention but completed most subsequent assessments.”
There was no evidence that this treatment increased substance use, and for participants overall there was unchanged in AUDIT or DUDIT scores overall.
The study raised some specific concerns:
They note moderate-high episodes of elevated blood pressure coinciding with anxiety symptoms during the psilocybin session, which could be a concern for a population with hypertension. Further evidence that the benefit of care in a medical setting.
Given their experience with their participants, they urge caution with borderline-personality disorder and the need for specialized training due to the unique risks of this population.
This study also illustrates a less homogenous population with medical issues, drug use and maybe personality disorders. What’s going to happen to that population that dissociates very easily (like borderline personality disorder)? If this person has a history of psychosis, bipolar, or personality disorder we don’t know what would happen at this point, so more studies are needed.
Secondary effects and experiences
Acute, subacute and long-term subjective effects of psilocybin in healthy humans: a pooled analysis of experimental studies.(Studerus et al., 2011)
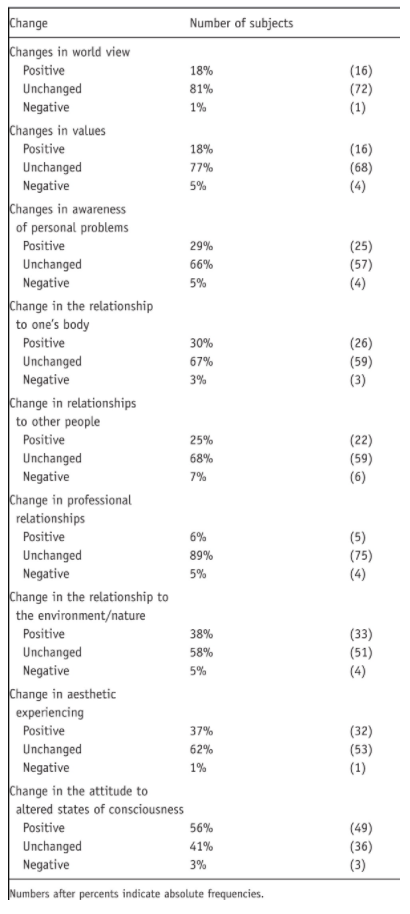
Study Size: This is study of 110 overall healthy individuals getting a total of 227 doses from low to high-doses.
Outcomes: With the study population they asked them to rate their subjective experiences with results below.
Personality
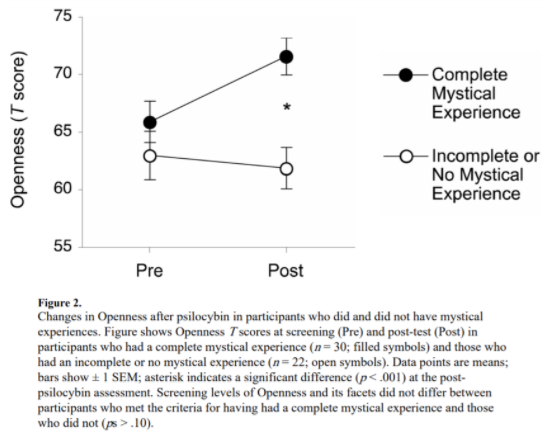
Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness.(MacLean et al., 2011)
Openness is defined as acceptance of new ideas and values, imagination, aesthetic appreciation, novelty-seeking, non-conformity, and creativity.
Participants: 52 Hallucinogen naive participants between 2 studies
Results: Significant increases in openness that remained over a year after session as measured by a NEO-PI T-score with increased average openness of 4 points after high-dose psilocybin and maintained for a year after the session, with a p value of 0.023
This is a change of just under half a standard deviation, which while it is not particularly clinically impressive, the article points out that it can cause some personality change, and is the only discrete measured experimental condition that has been shown to increase openness.
For more on openness, view our prior episode: Episode 098: The Big Five: Openness
There were no significant changes in Conscientiousness, Extraversion, Agreeableness or Neuroticism.
As has been seen in a lot of these studies, the change in openness is mediated by mystical experience.
Limitations: The population was highly educated and spiritually active, which may limit the generalizability of the study. Additionally, the participants’ level of neuroticism was on average 1 SD below normal at the start of the study, which may indicate ceiling effects.
Adam Borecky M.D. (a colleague of mine working on an ethics paper on psilocybin) wondered whether we should give informed consent that your personality may change due to psilocybin use. Interestingly, those who did not have a mystical experience during their use did not have a shift in openness, but those who did feel it was a mystical experience had a bigger shift. Thus, there is potential for anyone who has a mystical experience while taking psilocybin to increase their openness half a standard deviation. Should medical professionals be required to have informed consent for such an outcome? If your partner is higher openness than you, it might actually be a good thing to be a little more open. I have found that large discrepancies in openness between partners can create conflict.
There was one study that looked at whether certain types of therapies could change openness. They found that there was one study (Jackson 2012) which was an inductive reasoning training and they found it was possible to increase openness. So, there are other things that could potentially change openness as well. If you were giving inductive reasoning type of training, you probably wouldn’t ask for consent for a shift in openness, but it is something to think about. Your personality may change permanently. It’s not a huge change from just one dose, but it may change.
Effects of psilocybin therapy on personality structure (Erritzoe et al., 2018)
Population: 20 patients with moderate-severe depression
Results: From baseline to 3-month followup, the NEO-PI-R ‘Big Five’ score of Neuroticism significantly decreased, Extraversion and Openness scores significantly increased, Conscientiousness showed a trend-level increase, and no changes were seen in agreeableness.
In this study they showed, specifically with openness, about the same half a standard deviation increase. In neuroticism they showed a little more than a half a standard deviation decrease which is good because you want to decrease neuroticism. Any good treatment, whether it’s psychotherapy or medications, will decrease neuroticism.
When compared to traditional pharmacological treatment of depression (SSRI, SNRIs, etc.), changes in Neuroticism (0.57 vs 0.59), Agreeableness (0.04 vs 0.01), and Conscientiousness (0.18 vs 0.27) scores were very similar to this study
In contrast, effect sizes for Openness in this trial (which were already higher than average) were more than 3 times larger (0.44 vs. an average of 0.13) and more than 2 times larger for Extraversion (0.72 vs. 0.32) than the average effect sizes from the trials with antidepressant medications.
In this paper, they did a review of more than 200 studies and concluded that enduring and large changes in personality are obtainable through a range of therapeutic interventions, but none can do it as quickly or with the same magnitude as with psychedelics.
Limitations: Relatively small sample size of 20 patients suffering treatment-resistant depression. This was an open-label design with no control condition.
Personal meaning and spiritual significance
Psilocybin-occasioned mystical-type experience in combination with meditation and other spiritual practices produces enduring positive changes in psychological functioning and in trait measures of prosocial attitudes and behaviors (R. R. Griffiths et al., 2018)
Participants: 75 total healthy participants
Methods: participants were split evenly between three study conditions: (1) low-dose (active placebo) psilocybin with moderate-level (“standard”) support for spiritual practice; (2) high-dose psilocybin with standard support; and (3) high-dose psilocybin with high support.
Standard support (total of 7 hrs 20 minutes) with 5 hrs of preparation to build rapport, prepare for experience before psilocybin, and one hour the day following each session and 10 minutes two weeks after each session
High support (total of 35 hrs), 10 hrs pre-session, 3 hrs between sessions, 10 hrs individual sessions, followed by group therapy for ~12 hrs.
Results: There were increases in personal meaning, spiritual satisfaction, well-being, life satisfaction, life meaning/purpose, gratitude, interpersonal closeness, forgiveness, and death transcendence which were sustained at 6 month followup.
The impact of therapy makes a difference with life meaning, forgiveness, mysticism, and when people rate their lives as scared or spiritual.
Like other studies, mystical experience appeared to mediate the change. This study did not find significant changes in the Big Five as measured by NEO-PI.
Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later (R. Griffiths et al., 2008)
This study was conducted to gain greater understanding of the spiritual/mystical experience associated with the experience.
Participants: 36 healthy, hallucinogen-naïve adults reporting regular participation in religious/spiritual activities such as religious services, prayer, meditation, or study groups. Participants were low on Neuroticism (T-score 41.8) and high on Extroversion (55.3), Openness (65.7), and Agreeableness (55.7); low on Negative Affect on the PANAS-X (44.4); and high on the Measure of Actualization Potential (59.2), Mysticism Scale-Lifetime (55.6), and Spiritual Transcendence Scale (63.1)
Methods: 8 hours of preparation for the psilocybin experience. There were three sessions with two sessions of methylphenidate 40 mg/70kg and one session of psilocybin 30 mg/kg to compare the different effects.
Results: At the 14-month follow-up, 58% rated the psilocybin-occasioned experience as being among the five most personally meaningful and 67% rated it as among the five most spiritually significant experiences of their lives; 64% indicated the experience increased well-being or life satisfaction; 58% met criteria for having had a “complete” mystical experience; 61% rated that the experience was associated with moderate to extreme positive behavior change
Limitations: The study population was demographically homogeneous.
These participants described the mystical experience in various ways:
Theoretical explanation of the additive effects combining therapy with psilocybin
Depression, Mindfulness, and Psilocybin: Possible Complementary Effects of Mindfulness Meditation and Psilocybin in the Treatment of Depression. (Heuschkel & Kuypers, 2020)
Neurological effects
Psychedelics Promote Structural and Functional Neural Plasticity (Ly et al., 2018)
Methods: Studied the effect that DOI (an amphetamine substitute for MDMA), LSD (an ergoline psychedelic), DMT (a tryptamine analogue psychedelics) had on neuronal growth compared to placebo (VEH). They used neurons from fruit flies (drosophila) during both early stage and more mature development, zebrafish, as well as rat cortical neurons.
Results: In non-human models, psychedelics can stimulate neuroplasticity and neurogenesis with increases in BDNF, dendritic growth, and increased synaptic connectivity through 5HT-2a, TrkB-and mTOR-dependent mechanisms.
This showed that the neuronal stimulation occurs through an evolutionarily conserved mechanism. This appears to occur through 5HT-2A agonism, because when they used ketanserin, a 5HT-2a antagonist, the effects were similar to the control condition.
We know that there are other things like exercise and diet that can increase BDNF (Brain Derived Neurotrophic factor) which is like Miracle-Grow for the brain. In this study psilocybin increased that as well.
The next few studies look at fMRI imaging, often focused around a recognized functional neuronal circuit called the default mode network: (“Default Mode Network,” 2020)
Wikipedia: “[The default mode network is] a large-scale brain network primarily composed of the medial prefrontal cortex, posterior cingulate cortex/precuneus and angular gyrus. It is best known for being active when a person is not focused on the outside world and the brain is at wakeful rest, such as during daydreaming and mind-wandering.”
In Michael Pollan’s book “How to Change your Mind”, he describes the default mode network as our personal “orchestra conductor”, involved in self-reflection, self-criticism, and when we function on auto-pilot. It is involved in “time travel” (thinking about future or past), theory of mind, experiential or autobiographical self often narrating our experience. It also functions as our cognitive “circuit board”, keeping out things that are threatening us, suppression of subconscious thoughts or emotions and as a result of this cuts off parts of unconscious experiences.
Hyperconnectivity of DMN has been implicated in the “hyper-stability”/“rigidity” of the brain in depression, anxiety, addiction, OCD, anorexia disorders.
Of note, brain imaging studies are somewhat limited and study brain functioning often by looking at fMRI BOLD signals, which is a measure of de-oxygenation in the brain. The assumption is that it indicates more neuronal activity, but that is not necessarily the case.
Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. (Robin L. Carhart-Harris et al., 2012)
Results: This study found that stimulation of the 5HT-2a receptor by psilocybin led to acute decrease in activation of the mPFC (anterior cingulate cortex), Thalamus and posterior cingulate cortex. These effects appear to decrease the connectivity of the thalamus and associated default mode network.
Down-regulation of the default-mode network and related structures is central to the psychedelic experience and therapeutic benefit, and is associated with increases in openness and cognitive flexibility.
Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms.(Robin L. Carhart-Harris et al., 2017)
Population: 19 patients with treatment resistant depression.
Methods: No psychotherapeutic intervention. fMRI imaging was done pre-treatment and one day post-treatment.
Results: All patients showed some decrease in depressive symptoms, 12 participants meeting criteria for response. 9 participants showed continued response at 5 weeks with 6 participants in remission.
This study suggested that psilocybin use changes amygdala reactivity. Post-treatment, they recorded increased amygdala activation when emotional stimuli were presented and attenuated amygdala activity at rest. They note that both outcomes would be expected in successful depression treatment due to reduced emotional blunting.
They were surprised to find increased default mode network resting-state functional connectivity was greatest in individuals who maintained treatment-response at 5 weeks. The authors contend that their results could be representative of a similar mechanism of action of electroconvulsive therapy, where connectivity of the default more network is acutely disintegrated and then normalized post-treatment in a “reset” that facilitates subsequent changes.
Emotions and brain function are altered up to one month after a single high dose of psilocybin. (Barrett et al., 2020)
Participants: 12 healthy volunteers
Methods: An open-label pilot study using 25 mg/70 kg. With 2 preparatory session (for a total of 8hrs) and one follow up the day after the psilocybin experience. They tested cognitive function at baseline, one week after and one months after the psilocybin session.
Results: This study identified sustained effects of a single high dose of psilocybin on affect and the neural correlates of affective processing.
This study noted increases in openness, and decreases in neuroticism (although they do not provide an effect size), with measures of conscientiousness increased (d = 0.738) one month after administration of psilocybin.They found participants have increased responses in reward-learning, attention, and decision-making circuits.
In this study, there was initially a decrease in amygdala activity and negative affect in response to negative stimuli which returned to baseline after a month. In addition, they found a global increase in functional connectivity at both 1 week and 1 month post-psilocybin.
Effective connectivity changes in LSD-induced altered states of consciousness in humans (Preller et al., 2019)
Participants: 25 healthy adults
Methods: This was double-blind, randomized, placebo-controlled, cross-over study in 25 healthy participants who either received LSD or and LSD+ketanserin (a 5HT-2a antagonist). They used spectral dynamic causal modeling (DCM) for resting-state fMRI data looking at the cortico-striato-thalamo-cortical (CSTC) pathways.
Results: LSD alters effective connectivity within CSTC pathways: LSD selectively opens the thalamic filter to the posterior cingulate cortex and certain areas of the cortex. This is a fMRI imaging example of 5HT-2A agonist ‘loosening’ the experiential gating, allowing for more information processing and more experiential stimuli being experienced consciously.
While these studies aim to show the underlying mechanism of action of psychedelic mind-states, it is important to recognize purely neurobiological interpretations regarding brain activity during acute phases of a psilocybin experience can be reductionistic. These studies are unlikely to ever adequately capture the dynamics of a psychotherapeutic process that may unfold in the weeks or months that can foster enhanced meaning and greater well-being.
Theoretical mechanism of action discussion
REBUS (RElaxed Beliefs Under Psychedelics) and the Anarchic Brain: Toward a Unified Model of the Brain Action of Psychedelics. (R. L. Carhart-Harris & Friston, 2019)
This is a theoretical paper that hypothesizes that “psychedelics work to relax high-level priors, sensitizing them to liberate bottom-up information flow, which, with the right intention, care provision and context, can help guide and cultivate the revision of entrenched pathological priors.”
High-level priors or beliefs ordinarily have an important constraining influence on the default mode network, limiting the expression and influence and alternative ideas. An important example of a high-level prior is the belief that one has a particular personality and set of characteristics and views.
By relaxing high-level priors or beliefs (eg. depression) under psychedelics, it allows bottom-up experiences that would otherwise be filtered out to be experienced consciously. At low doses this leads to a disruption in visual experience, and at higher doses it can lead to dissolving of ego boundaries and a “unitive experience” (a sense of union and interconnectedness with objects and entities previously seen as external to oneself).
This is how therapy works to some degree. You have a person in connection with you that decreases shame experience over and over again. The therapist's action to decrease the internal critic and internal shame that a patient feels is paramount for any therapy to work. This is what separates the best therapists from the moderately good therapists. How well do you reduce that shame experience? Maybe that has to do with decreasing the critical parts of the frontal lobe.
As a word of caution, They warn that if rates of psychedelic use were to escalate, people who have poorly integrated experiences (prevalent with people with psychotic experiences) could lead to increased uncertainty that can lead people to seek explanation through delusional beliefs that serve to stop-gap uncertainty.
This is similar to what was being hinted at earlier regarding whether or not there are things being connected that shouldn‘t be. Think about the high-stress environment that we are in at the moment with COVID-19, political unrest, political divisions that are more polarized than ever before. In order for people to maintain what makes sense of the world, they may be jumping to connect things that are not connected. Part of the problem with a new treatment like this is that when it is done, it is usually done on people who have moderate depression who don’t have personality conflicts such as disorganized attachment or borderline personality disorder. Then when this gets out into the mainstream it will be given out to everyone indiscriminately (by some people). Some people who are opening Ketamine treatment centers right now aren’t psychiatrists or therapists. Similarly, they may not have the selection criteria to determine who should receive psilocybin treatments and who shouldn’t.
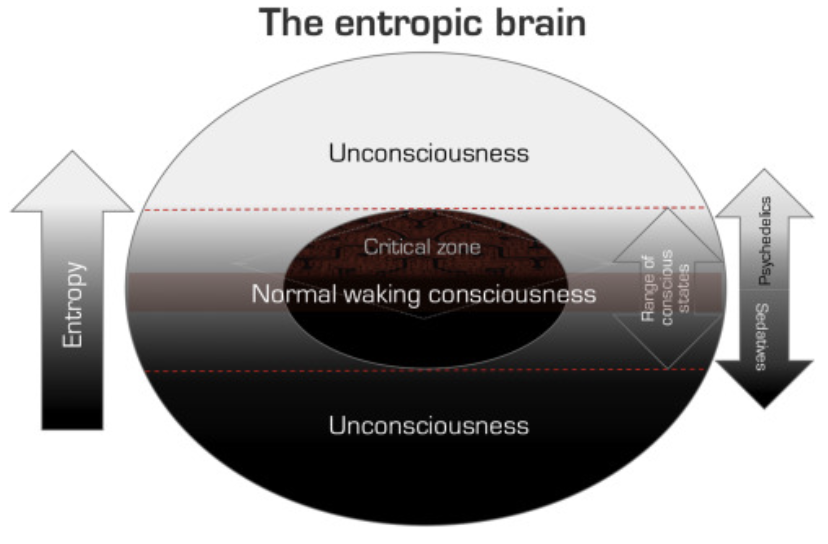
The entropic brain - revisited (Robin L. Carhart-Harris, 2018) and Serotonergic psychedelics LSD & psilocybin increase the fractal dimension of cortical brain activity in spatial and temporal domains (Varley et al., 2020)
These papers are heavily influenced by basic principles of information theory and more specifically, the notion that the entropic brain maintains that uncertainty and information content are near equivalents and that entropic-brain-states are experienced as content-rich, but at the same time, are unpredictable and uncertain.
They note that there are increasing levels of entropy in the brain in different states of consciousness, namely vegetative states, coma, sedation/anesthesia, sleep, awake, and under the influence of psilocybin/LSD.
They compare this to the creative process when there are lots of disorganized ideas (initial entropic state) that is exploratory and divergent in nature which is then followed by more protracted processes of cognitive convergence.
Systematic reviews
Long-term effects of psychedelic drugs (psilocybin, LSD): A systematic review.(Aday et al., 2020)
Studies reviewed: depressed individuals (10 studies), healthy volunteers (9 studies), those with end-of-life distress (7 studies; many of which were also depressed/anxious), tobacco use disorder (4 studies), spiritually active individuals (2 studies), alcohol use disorder (1 study), and meditators (1 study).
Conclusions:
Seven distinct studies examined lasting changes in openness to experience. Participants reported increases in four of the studies. They note that the participants in the studies were already high in openness prior to the experiment, potentially indicating ceiling effects.
All nine studies assessing changes in wellbeing/quality of life showed improvements.
Of the ten studies assessing long-term changes in spirituality after psychedelic use, nine found increased ratings.
All four studies examining psilocybin-assisted psychotherapy for substance use disorders (three tobacco use disorder and one alcohol use disorder) demonstrated positive abstinent effects at the group-level
Psychedelics and Psychedelic-Assisted Psychotherapy (Reiff et al., 2020)
Studies reviewed: Seven different psilocybin clinical trials.
In their conclusion they support continued research and investigation, but do not support clinical use outside of research at this time. To support this, they note improvements in depression, anxiety substance for weeks to months with only a few sessions, with better results than other treatments
The review article cited several concerns, including concerns about the limited ability for these studies to do adequate blinding. They also noted the importance of therapy in the protocols and inconsistencies in how therapy is done in different studies.
The journal’s editorial noted additional concerns about the specific indications that psilocybin should be used for. They note that many studies used broad diagnostic criteria, so they wonder which patients would most benefit? How severely ill they should be? If “walking worried” or patients with subsyndromal illness, or patients with milder depressive or anxious symptoms would benefit?
We note some limitations of the psychiatric community, how the research community is often focused on DSM diagnoses, but the differences clinically might not be as significant.
Additionally, it is different for scientists to measure mystical experiences, personality changes, the experiential component of the experience can often be perceived as a unnecessary/unwanted/undesirable side effect, but in these studies, the mystical experience appears to be a crucial component of the therapy and a mediator of the beneficial components of the experience.
It should be noted that the medical community has ended up prescribing medication that have resulted in societal issues. This has historically occurred with opioids, benzodiazepines, and Z-drugs which had addictive side effects that were not initially recognized. There is ongoing concern that the recent increased prevalence in ketamine clinics will result in similar side effects long-term. This has resulted in a psychiatric community that is conservative about new medications that might end up being drugs of abuse. Of note, as discussed in Part 1, this is not as much as concern with psilocybin.
Future of study
In late 2018, psilocybin was designated by the United States Food and Drug Administration as a “breakthrough therapy” for treatment-resistant depression. This process expedites the development and review of psilocybin due to preliminary clinical evidence that indicates that the drug has substantial improvement over available therapy.
In the 2020 election, in Oregon, Measure 109 passed. This resulted in the decriminalization of plant and synthetic psilocybin and established a two-year development period to create the groundwork of making program for administering psilocybin products, such as psilocybin-producing mushrooms and fungi, to individuals aged 21 years or older at a “psilocybin-service center”.
The therapy will require preparation, supervision during the session and integration sessions and would be available to anyone that it is not contraindicated for.
There are a number of companies pursuing psilocybin research:
Compass pathways is a Public traded for-profit company, with investors, backed by Peter Thiel . They are conducting a randomised controlled phase IIb study of psilocybin therapy in 216 patients with treatment-resistant depression in 20 sites across Europe and North America.
Usona Institute is a non-for-profit company conducting a 80 participant randomized-controlled trial for major depressive disorder. Sites and principal investigators participating in the study include: Johns Hopkins University (Roland Griffiths, PhD), NYU School of Medicine (Stephen Ross, MD), University of California San Francisco (Joshua Woolley, MD, PhD), Yale University (Gerard Sanacora, MD, PhD), University of Wisconsin-Madison (Randall Brown, MD), Great Lakes Clinical Trials (Rupal Trivedi, MD) in Chicago, and Segal Trials (Rishi Kakar, MD) in Miami.
Currently, there are a number of studies that are either ongoing or recruiting participants: Current studies
Johns Hopkins University’s Center of Psychedelic and Consciousness Research have ongoing studies: Depression, Smoking Cessation, Alzheimer’s and Anorexia Nervosa.
Ongoing European Studies on fMRI imaging, attention/cognition, and visual changes
Other studies that future, ongoing or completed: Healthy volunteers exploring the experience, depression, anxiety, cluster headaches, cocaine use, alcohol use, opioid use, and OCD.
Conclusions
As we have seen with the clinical trials, conducting randomized-control trials without confounders is particularly difficult when studying a substance that alters consciousness. Concerns about results will continue to prevail without a good control group, as a waitlist is likely to have a nocebo effect, and the therapy itself is susceptible to selection bias, expectation bias, attrition bias. It is possible that the best we can do is to ensure that we are creating an option that appears to provide benefit and can be done safely, which has been increasingly shown. Large trials will continue to be helpful, and the evidence seems to indicate that psilocybin can be administered safely.
Researchers continue to explore the therapeutic benefits of psilocybin, while the legal restrictions around its use continue to change. The evidence reviewed supports that psilocybin be rescheduled to a schedule 4 substance, and similar to other substances in this class, should probably be decriminalized. How psilocybin therapy will be conducted, and who will have prescribing capabilities, will need to be determined. Currently, there are organizations developing training programs, but there is an open question about it being vulnerable to regulatory capture and access to the overall population.
The preliminary and phase 2 clinical trials and secondary effects discussed here show that the psilocybin-assisted psychotherapy is a promising treatment for mood disorders, anxiety, substance use and beyond. The limitation of these studies notwithstanding, the results are impressive with 60-80% response and remission of anxiety and depressive disorders, and 50-80% improvement with substance use disorders. Psilocybin has demonstrated its ability to generate rapid but moderate shifts in personality, changes in brain fMRI imaging both acutely and for weeks after a psilocybin experience. It has been suggested, and remains to be seen if it is also well-suited for other mental conditions marked by rigid, compulsive processes of thought and behavior, which can include eating disorders. It will be interesting to consider a study looking at comparing psilocybin therapy to current excellent care, like day treatment programs.
The secondary effects of these treatments demonstrate that people overwhelmingly find the experience among the most significant and meaningful of their lives. The ability to help create meaning within a therapeutic process is critically important, and can be particularly useful for those experiencing challenges around existential questions, grief, and palliative care, where otherwise the psychopharmacological toolkit is limited.
References
Drug Toxicity. (2012, February 20). Robert Gable. https://rgable.wordpress.com/drug-toxicity/